This is online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputsThis e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
Hyndavi Konakanchi, Intern
7/1/23
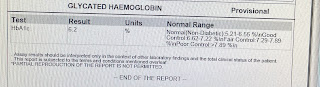
A CASE DISCUSSION OF 62/M ON TYPE 1 RESPIRATORY FAILURE WITH HEART FAILURE WITH K/C/O CKD WITH K/C/O HTN , DM TYPE 2 & OHA INDUCED HYPOGLYCEMIA
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Following is the view of my case :
Chief complaints : Difficulty in breathing since yesterday morning
Patient was apparently asymptomatic since 30 years. He then had burning sensation in feet and went to hospital. Necessary investigations were done and diagnosed with diabetes mellitus 2 and hypertension .with 150/100mmhg On metformin for 27 years , amlodipine 10mg
Burning sensation of feet and fatigue went to hospital at Nalgonda again three years ago . Was advised insulin. 30u morning and 15u night used for one year still uncontrolled diabetes so changed to mixtard 25u morning and 20u at night, later changed to 20u morning and 15u night since 2 years . Along with insulin also added gliclazide extended release tablets 60mg (recluse-XR 60) but defaulter.
Five years ago had UTI renal calculi post surgery was uneventful. Post surgery 8 months Investigations showed increase in creatine levels 1.6-2.0. Tab.uremax & Tab nodosis(sodium bicarbonate )500mg -2000mg per day on increased creatine levels >2.<2 1000mg ; He used these medicines - for 5 months when his creatinine level came to normal levels then he discontinued for 1 month; again when his creatinine was deranged he continued the medication again
Three years ago left hand weakness mouth deviation slurred speech mri brain was done and medications were given
Attacks of giddiness , unstable gait, swaying gait and slurred speech came to kamineni neuro opd MRI brain was done in 2021. ?hemorrhagic clot and medicines were prescribed.
Two years ago had an episode of epilepsy due to ?hypoglycemic episode was advised Ecospirin 150/70mg H/S.
Bilateral pedal edema pitting type present, burning micturition, decreased urine output, SOB grade 4 spo2 75% at room air. Fever at night not associated with chills and rigor , relived after one hour on taking Dolo 650mg taken , after one hour again had episode of fever, relived after one hour of taking Dolo 650mg. Cough with expectoration present.
Left limited mobility and pain on shoulder movement.
MEDICAL HISTORY:
* he is under medication ( MET XL - metoprolol and inj. Human mixtard , tab. Aspirin, tab. Clopitab )
Not a K/C/O asthma / Ischemic heart disease / epilepsy / TB
FAMILY HISTORY
No significant family history
PERSONAL HISTORY
OCCUPATION : Retired govt employee
DIET : Mixed
APPETITE : Normal
SLEEP : Normal
BOWEL AND BLADDER HABITS : Normal
ADDICTIONS: No
GENERAL EXAMINATION
* Patient is concious coherent and coperative, well oriented to time palce and person
* Built - moderately built , moderately nourished
VITALS
Blood pressure : 130/60 mm hg
Pulse Rate : 95 bpm
RR : 35 cpm
Temperature : 99.5 degrees F
SPO2 : at presentation 75% under RA &
91% under 8L of O2
EDEMA OF FEET : PRESENT ; PITTING TYPE
* NO PALLOR,ICTERUS , CYANOSIS, CLUBBING , LYMPHADENOPATHY
SYSTEMIC EXAMINATION
RESPIRATORY SYSTEM :
Inspection : bilateral symmetrical chest
Palpation: trachea centrally placed, bilateral symmetrical chest movements
Percussion: resonance
Auscultation: diffused wheezes and crepts in left and right sides of chest
PER ABDOMEN :
Inspection: distended
Palpation :soft non tender
Auscultation: bowel sounds heard
Percussion: shifting dullness present
CVS:
S1 S2 heard, JVP raised
CNS:
no focal deficit
INVESTIGATIONS:
6/1/23
7/1/23
8/1/23
9/1/23
10/1/23
On 6/1/23
On 11/1/23
Link to 2d echo :
TYPE 1 RESPIRATORY FAILURE WITH CARDIOGENIC PULMONARY EDEMA WITH K/C/O CKD WITH K/C/O HTN + , DM TYPE 2 + & OHA INDUCED HYPOGLYCEMIA
Restriction of fluid < 1.5 lts/ day
Restriction of salt < 2 gm/day
Inj.lasix 40 mg Iv/bd
Intermittent CPAP
Salbutamol nebulization 8th hrly
T.Nodosis 500 mg po/bd
T.Shelcal 500 mg po/bd
T.Carvedilol 3.125mg po/bd
Cap.Bio d3 po/OD weekly once
HAI acc to grbs
SOME OF MY LEARNING POINTS :
HOW ARE PT, INR TESTS DONE IN OUR LAB :
First blood of the patient is collected in blue coloured vacutainer ( containing an anticoagulant- 3.2% sodium citrate) and then blood is centrifuged for 15 mins thereby separating the plasma from the cells
MACHINE USED FOR CENTRIFUGE
SERUM SEPERATED FROM CELLS AFTER CENTRIFUGING
This plasma ( a quantity of 200 micro litres ) is taken into a tube and a quantity of 200 micro litres of reagent ( UNIPLASTIN - contains liquid rabbit brain thromboplastin ) is taken into an other tube ; now both tubes are kept in water bath ( of temp 37 degree celsius )— wait for 3 mins
REAGENT : UNIPLASTIN
WATER BATH
After 3 mins ; take both tubes out of water bath and then start a timer & add patient’s plasma to reagent ; the time by which clot formed is noted and is determined as PT ( the time in seconds is counted manually )
The normal range of PT is 10-16 seconds
Coming to INR ; it is calculated by dividing patient’s PT with control PT ie., INR = PATIENT’S PT / CONTROL PT
Control PT is standard value ( constant ) which is 13.5 seconds
The normal range of INR is less than 1 , any value higher than 1 is considered as significant derangement; but jn patient’s using warfarin ; INR of a range of 2-3 is considered normal
Dr Shailesh presentation on case of complex diabetes.
QUESTIONS ASKED :
1) How do you diagnose cardiogenic pulmonary edema?
2) What is the treatment difference in cardiogenic pulmonary edema and non cardiogenic pulmonary edema?
3) How much duration will it take to cause macroangiopathy?
4) How will Diabetes cause heart failure?
SOAP NOTES :
7/1/23
Unit 5
Dr Hyndavi, intern
Dr Akash, intern
Dr Himaja, PGY1
Dr Pavani, PGY2
Dr Sai charan PGY3
Dr Abhinaya SR
ICU BED 5 DAY 2
62/M
S:
SOB
B/L pedal edema
Productive Cough
O:
Pt is c/c/c
Temp:98.2 F
PR: 102 bpm
RR: 24 cpm
Spo2 : 92 @ 4 lts O2
Grbs : 184 mg/dl
I/O : 600/1000 ml
CVS: S1,S2 + , JVP rised
RS: BAE +, Rt inframammary crepts + wheeze + & lt inframammary crepts +
P/A: distended, soft , non tender, BS + & shifting dullness +
CNS : NFND
A :
TYPE 1 RESPIRATORY FAILURE WITH CARDIOGENIC PULMONARY EDEMA WITH K/C/O CKD WITH K/C/O HTN + , DM TYPE 2 + & OHA INDUCED HYPOGLYCEMIA
P:
Restriction of fluid < 1.5 lts/ day
Restriction of salt < 2 gm/day
Inj.lasix 40 mg Iv/bd
Intermittent CPAP
Salbutamol nebulization 8th hrly
T.Nodosis 500 mg po/bd
T.Shelcal 500 mg po/bd
T.Carvedilol 3.125mg po/bd
Cap.Bio d3 po/OD weekly once
Inj.piptaz 225 mg IV/TID
HAI acc to grbs
8/1/23
Unit 5
Dr Hyndavi, intern
Dr Akash, intern
Dr Himaja, PGY1
Dr Pavani, PGY2
Dr Sai charan PGY3
Dr Abhinaya SR
AMC BED 2 , DAY 3
62/M
S:
Stools not passed
Sleep -
Productive Cough +
SOB +
Fever spikes -
O:
Pt is c/c/c
BP: 130/60 mm Hg
PR: 78 bpm
RR: 16 cpm
Spo2 : 85 %@ RA
Grbs : 125 mg/dl
I/O : 650/1100 ml
CVS: S1,S2 + , JVP not rised
RS: BAE +, lt side crepts + & diffuse wheeze +
P/A: distended, soft , non tender, BS + & shifting dullness +
CNS : NFND
A :
TYPE 1 RESPIRATORY FAILURE WITH CARDIOGENIC PULMONARY EDEMA WITH K/C/O CKD WITH K/C/O HTN + , DM TYPE 2 + & OHA INDUCED HYPOGLYCEMIA
P:
Restriction of fluid < 1.5 lts/ day
Restriction of salt < 2 gm/day
Inj.lasix 40 mg Iv/bd
Intermittent CPAP
Salbutamol nebulization 8th hrly
T.Nodosis 500 mg po/bd
T.Shelcal 500 mg po/bd
T.Carvedilol 3.125mg po/bd
Cap.Bio d3 po/OD weekly once
Inj.piptaz 225 mg IV/TID
HAI acc to grbs
Syrup Cremaffin 15ml po/Tid
9/1/23
Unit 5
Dr Hyndavi, intern
Dr Akash, intern
Dr Himaja, PGY1
Dr Pavani, PGY2
Dr Sai charan PGY3
Dr Abhinaya SR
AMC BED 2 , DAY 4
62/M
S:
Stools not passed
Sleep +
Productive Cough +
SOB decreased
Fever spikes -
O:
Pt is c/c/c
BP: 130/70 mm Hg
PR: 78 bpm
RR: 18 cpm
Spo2 : 94%@ RA
Grbs : 181 mg/dl
I/O : 1000/1050 ml
CVS: S1,S2 +
RS: BAE +
P/A: Soft, tender(diffuse)
CNS : NFND
A :
TYPE 1 RESPIRATORY FAILURE WITH CARDIOGENIC PULMONARY EDEMA WITH K/C/O CKD WITH K/C/O HTN + , DM TYPE 2 + & OHA INDUCED HYPOGLYCEMIA
P:
Restriction of fluid < 1.5 lts/ day
Restriction of salt < 2 gm/day
Inj.lasix 20 mg Iv/bd
Intermittent CPAP
Salbutamol nebulization 8th hrly
T.Nodosis 500 mg po/bd
T.Shelcal 500 mg po/bd
T.Ultracet po /Qid
T.Carvedilol 3.125mg po/bd
Cap.Bio d3 po/OD weekly once
Inj.piptaz 225 mg IV/TID
HAI acc to grbs
Syrup Cremaffin 15ml po/Tid
10/1/23
Unit 5
Dr Hyndavi, intern
Dr Akash, intern
Dr Himaja, PGY1
Dr Pavani, PGY2
Dr Sai charan PGY3
Dr Abhinaya SR
DAY 4
62/M
S:
Stools passed
Sleep +
Productive Cough decreased
No SOB
Fever spikes -
O:
Pt is c/c/c
BP: 130/80 mm Hg
PR: 74 bpm
RR: 20 cpm
Spo2 : 94%@ RA
CVS: S1,S2 +
RS: BAE +
P/A: Soft, non tender
CNS : NFND
A :
TYPE 1 RESPIRATORY FAILURE WITH COMMUNITY ACQUIRED PNEUMONIA WITH K/C/O CKD WITH K/C/O HTN + , DM TYPE 2 + & OHA INDUCED HYPOGLYCEMIA
P:
Restriction of fluid < 1.5 lts/ day
Restriction of salt < 2 gm/day
Intermittent CPAP
Salbutamol nebulization 8th hrly
T.Nodosis 500 mg po/bd
T.Shelcal 500 mg po/bd
T.Ultracet po /Qid
T.Carvedilol 3.125mg po/bd
Cap.Bio d3 po/OD weekly once
Inj.piptaz 225 mg IV/TID
HAI acc to grbs
Syrup Cremaffin 15ml po/Tid
11/1/23
Unit 5
Dr Hyndavi, intern
Dr Akash, intern
Dr Himaja, PGY1
Dr Pavani, PGY2
Dr Sai charan PGY3
Dr Abhinaya SR
DAY 5
62/M
S:
Stools passed
Sleep +
Productive Cough decreased
No SOB
Fever spikes -
O:
Pt is c/c/c
BP: 120/80 mm Hg
PR: 72 bpm
RR: 20 cpm
Spo2 : 94%@ RA
Grbs : 152 mg/dl
CVS: S1,S2 +
RS: BAE +
P/A: Soft, non tender
CNS : NFND
A :
TYPE 1 RESPIRATORY FAILURE WITH COMMUNITY ACQUIRED PNEUMONIA WITH K/C/O CKD WITH K/C/O HTN + , DM TYPE 2 + & OHA INDUCED HYPOGLYCEMIA
P:
Restriction of fluid < 1.5 lts/ day
Restriction of salt < 2 gm/day
Intermittent CPAP
Salbutamol nebulization 8th hrly
T.Nodosis 500 mg po/bd
T.Shelcal 500 mg po/bd
T.Ultracet po /Qid
T.Carvedilol 3.125mg po/bd
Cap.Bio d3 po/OD weekly once
Inj.piptaz 225 mg IV/TID
HAI acc to grbs
Syrup Cremaffin 15ml po/Tid



































Comments
Post a Comment