This is online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputsThis e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
Hyndavi Konakanchi, Intern
3/1/23
A CASE DISCUSSION 60/F CASE WITH CRF WITH DM, HTN & OLD CVA
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Following is the view of my case :
Pt came to opd with cheif complaints of swelling in the limbs since 4 months , SOB and lower back pain since 1 day
Pt was apparently asymptomatic 10 yrs ago and the. She developed DIABETES , later after 1 yr she developed HYPERTENSION
SHE WAS ON REGULAR MEDICATION SINCE THEN
Interesting history of the patient; 5 yrs back one fine day she developed headache, giddiness, vomitings for which she was taken to nalgonda govt hospital; she was dmitted for nearly 8 days ; CT SCAN was done during this time and she was diagnosed to have post parietal infarct with chronic lacunar infarcts ; and was kept on medications since then ; she is using them continuously till now
2 yrs before ; she had B/L limb weakness — went to hospital ; doctor told her sugar levels are not controlling and kidney was affecting ; from then she did dietary modification & used regular medications
4 months ago ; when she is doing her household activity she noticed B/L limb swelling( B/L pedal edema ); then she went to some hospital; there doctor advised medications, dietary modifications and some physical activity , pt had followed them ; slowly limb swelling came down and pt started feeling better…
Everything was fine until 29/12/31 then she developed SOB ( grade 4) without doing any activity and pt felt her limb swelling ( B/L pedal edema ) was also increased so she came to our hospital for that
COMING TO HER DAILY ROUTINE: She is a housewife
She wakes up at 6am in the morning — freshen up & does house hold activities
She eats lunch at 1 pm and sleep for a while
She wakes at 5 pm and she does house hold activities , have dinner at 8 pm and goes to sleep by 10:30 pm
She eats breakfast in the morning, rice and curry in theafternoon, night
But after she was diagnosed to have kidney diesease ; she started to consume food which is less salty,spicy,oily and decreased water intake
MEDICAL HISTORY:
* She is under medication ( MET XL - metoprolol and inj. Human mixtard , tab. Aspirin, tab. Clopitab )
Not a K/C/O asthma / Ischemic heart disease / epilepsy / TB
FAMILY HISTORY
No significant family history
PERSONAL HISTORY
OCCUPATION : House wife
DIET : Mixed
APPETITE : Normal
SLEEP : Normal
BOWEL AND BLADDER HABITS : Normal
ADDICTIONS: No
GENERAL EXAMINATION
* Patient is concious coherent and coperative, well oriented to time palce and person
* Built - moderately built , moderately nourished
VITALS
Blood pressure : 140/80 mm hg
Pulse Rate : 99 bpm
Temperature : 98.6 degrees F
SPO2 : 98 @ RA
PALLOR : PRESENT
EDEMA OF FEET : PRESENT
* NO ICTERUS , CYANOSIS, CLUBBING , LYMPHADENOPATHY






SYSTEMIC EXAMINATION
CVS EXAMINATION
Inspection-
* The chest wall is bilaterally symmetrical
* No raised JVP.
Palpation-
* Apical impulse is felt in the left 5th intercostal space, medial to the midclavicular line
* No parasternal heave felt.
Percussion-*resonant note heard- no pericardial effusion
Auscultation-
## Mitral area , aortic area , pulmonary area
* S1 and S2 heard, no added thrills and murmurs are heard
PER ABDOMINAL EXAMINATION :-
Inspection:
* Abdomen is distended
* Umbilicus is inverted
Movements :
* Gentle rise in abdominal wall in inspiration and fall during expiration.
* No visible gastric peristalsis
palpation :
* SOFT, NON TENDER, NO ORGANOMEGALY
Percussion:
Resonant note heard
No fluid (ascitis)
Auscultation:
* Normal bowel sounds.
RESPIRATORY SYSTEM EXAMINATION :-
Inspection-
* Upper respiratory tract - Normal
* Shape of chest - elliptical & Bilaterally symmetrical
* Trachea- in midline
* no scars and sinuses
* no visible pulsations
* no engorged veins
* no usage of accessory respiratory muscles
Palpation-
* No local rise of temperature
* No tenderness
* All the inspectory findings are confirmed
* Apical Impulse :- 5th intercostal space 1 cm medial to mid clavicular line
* Trachea is in normal position.
* chest expansion - normal.
* Movements of chest with respiration are normal.
vocal fremitus - normal.
Ausclutation-
* Bilateral air entry - present.
* Normal vesicular breathsounds are heard.
* No advantitious sounds heard.
CNS EXAMINATION :-
* No focal neurological deficits
* Higher motor functions are normal
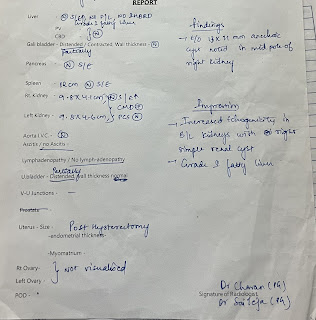
INVESTIGATIONS:
DIAGNOSIS :
CRF WITN HTN , DM WITH OLD CVA
TREATMENT:
1) TAB. LASIX 40 MG PO /BD
2) TAB. CLOPITAB A ( 75/20 ) PO/ H/S
3) TAB.NODOSIS 500 MG PO/BD
4) TAB.SHELCAL 100 MG PO/OD
5) CAP BIO D 3 PO/OD
6) INJ.ERYTHROPOIETIN 4000IU S/C WEEKLY ONCE AFTER HD
7) INJ.OROFER XT PO/OD
8) SALT RESTRICTION <1.5 gm / DAY & WATER RESTRICTION < 1.5 lts / DAY
9) INJ.IRON SUCROSE 100 MG + 100 ML NS IV WEEKLY ONCE
10) INJ.HAI S.C ACCORDING TO GRBS
11) CAP.LOBULIN FORTE PO/OD
12) SYP.CREMAFFIN 10 ML PO/BD
13) TAB.NICARDIA RETARD 10MG PO/TID
14) TAB.NIFIDIPINE 10 MG PO/BD
15) TAB.ECOSPIRIN AV (75/20) PO/HS
16) TAB.AMLONG 5MG PO/BD















Comments
Post a Comment