This is online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputsThis e-log book also reflects my patient centered online learning portfolio and your valuable inputs on comment box is welcome.
Hyndavi Konakanchi, 8th semester
Roll no: 63
October 22, 2021
A CASE DISCUSSION ON PRE-RENAL AKI SECONDARY TO DEHYDRATION with HYPOVOLEMIC SHOCK , DIABETIC / ALCOHOLIC KETOACIDOSIS ,WERNICKES ENCEPHALOPATHY,ACUTE HEART FAILURE & REFRACTORY METABOLIC ACIDOSIS
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Following is the view of my case :
CASE PRESENTATION:
A 45 year old female , who studied 2nd standard , married at age of 16 and mother of 3 children ,shop keeper( Liquor store& General store ) by occupation& who was proactive in her day-to-day activities came to casualty in an altered sensorium with CHEIF COMPLAINTS of….shortness of breath since 4 days - GRADE : 4 , Vomiting since 1 day, fever since 2 days , decreased appetite since 3 days
HISTORY OF PRESENT ILLNESS:
According to patients husband she was 3 rd degree relative to him , she was very active since childhood . As father is a toddy collector, she used to drink alcohol from her very young age of approximately 5-6 yrs , but inspite of this there is no impact on her day to day activities and relations with her family members
She is married at the age of 16 , her husband is the owner of the liquor store but inspite of that she is not having the habit of drinking alcohol .
HER ROUTINE :
wakes up at 4 am — do home related works by 9 am and manages shop till evening 6 pm and then spend some good time with her family —have dinner by 9 pm — sleep ( adequate sleep )
Her life went good till she developed cough , fever at the age of 37 , for which she was taken to some local hospital and was diagnosed to have TUBERCULOSIS, she took ATT MEDICATION for 6 months ,at this time her routine was impaired with having decreased appetite and she used take all day rest ; after that she recovered & her routine became normal …
At the age of 38 , she developed polyuria , polydypsia and was taken to some local hospital , there she was diagnosed to have diabetes and from then , she was on OHA , her routine routine didn’t change greatly though …
After her first child marriage , at her age of 40 ; some relative of her told that drinking alcohol will increase her overall well-being & appetite, it is the root cause for developing alcoholic habit in her ….
— from then she took alcohol many times …
One day she suddenly developed pain abdomen and was taken to local hospital; there she was diagnosed to have ; some liver disease and took medication for that …
She had many ( once in every 3-4 months ) binge drinking episodes of alcohol (whisky ) - 180 ml , she had a very specific pattern of drinking ie ., she doesn’t eat any food and drinks only alcohol for 3-4 days and many a times she develops ; SOB , vomiting and weakness and she used to take symptomatic treatment for that , at these episodes she used to be irritable , there used to be quarrels between her and husband and after the episode; she developed asthma 4 yrs back and there is acute exacerbation after the alcohol binge .She used to be normal again ….
One year back , she was diagnosed to have jaundice and got treated in outside hospital
The intermittent alcohol episodes continued , untill she had recent binge of alcohol that is continous alcohol intake for 1 whole week , she became unconscious , as no one is there in house ( her husband went to some family function ) she was noticed in unconscious state by her neighbour and was taken to hospital 1 ( there they couldn’t take up the case because of the level of severity) — from there she is taken to hospital 2 — finally to hospital 3 where she is getting treatment currently…
On presentation to hospital 3 she has altered sensorium, shortness of breath since 4 days - GRADE : 4 ( according to NYHA classification) ; it was not associated with orthopnea & paroxysmal nocturnal dyspnoea
Vomiting since 1 day ; (5-6 episodes) not projectile , non bilious , food particles as content and was associated with pain abdomen ,
fever since 2 days ; low grade fever & not associated with chills & rigors,
decreased appetite since 3 days
She couldn’t do any work now …
PERSONAL HISTORY:
* Appetite: decreased
* Diet: mixed
* Sleep : adequate
* Bowel and bladder movements: # Irregular bowel movements &
## Normal micturition
* Additions: * History of toddy intake since her 6 yrs of age & alcohol ( whisky ) intake 180 ml since 5 yrs intermittently
FAMILY HISTORY:
* Not significant
GENERAL EXAMINATION:
Patient is in altered sensorium
She is not oriented to time, place and person.
She is thinly built and poorly nourished.
*** Patient is in dehydration ( has lost skin turgor , sunken eyes & dry tongue )
VITALS:
Temperature: Afebrile
Pulse Rate: 121 beats per minute
Blood pressure: Not recordable
Respiratory Rate: 22 cycles per minute
SpO2: 73% on room air
GRBS : 254 mg %

No pallor
No Icterus
No Cyanosis
No Clubbing
No Lymphadenopathy
No Edema
SYSTEMIC EXAMINATION:
1) Respiratory system:
* Position of the trachea : central
* Chest is symmetrical and there are no chest deformities
** There is increase in rate and depth of breathing ( kussumal’s breathing ) # DYSPNOEA: present
* No wheeze, no crepts
* Bilateral air entry is present
* Normal vesicular breath sounds are heard
* Equal movements on both sides on respiration
2)CVS:
* S1 and S2 heart sounds are heard
*No murmurs
3) ABDOMINAL EXAMINATION:
* All quadrants of abdomen are moving equally with respiration
* Abdomen is soft & non-tender
* Bowel sounds are sluggish
4) CNS:
* No abnormality detected
INVESTIGATIONS:
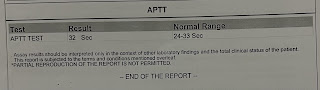
* HEMOGRAM, BLOOD GROUPING , URINE FOR KETONE BODIES , SERUM ELECTROLYTES , SERUM CREATININE, LFT ,ABG , CUE , 2D echo , CHEST X - RAY , ECG
Analysis of reports:
* URINE FOR KETONE BODIES WAS +ve
* HIGH ANION GAP IN ABG
* RENAL FUNCTION TESTS : ELEVATED CREATININE
DIAGNOSIS:
PRE-RENAL AKI SECONDARY TO DEHYDRATION with HYPOVOLEMIC SHOCK
DIABETIC / ALCOHOLIC KETOACIDOSIS
WERNICKES ENCEPHALOPATHY
ACUTE HEART FAILURE with EJECTION FRACTION : 45% ( may be secondary to shock )
# REFRACTORY METABOLIC ACIDOSIS ( here it is the indication for dialysis )
Known case of ASTHMA AND DIABETES
TREATMENT:
IVF 4 NS - bolus
Inj Nor adrenaline 8ml/hr ( 2amp in 47 ml NS)
IVF NS,RL @ 100 ml /hr continuos
Inj Sodium Bicarbonate 100meq /iv/ stat - 50 meq in 100 ml NS /IV / slow infusion over 2 hours
Inj PANTOP 40 mg /iv /od
Inj neomol 100ml /sos
Inj ZOFER 4mg /IV / OD
Inj Ceftriaxone 1 gm /iv/ bd
Inj HAI (39 ml NS with 40 IU HAI )
Inj Sodium Bicarbonate 1 amp in 100 ml NS /Stat
Inj Piptaz 4.5 gm /IV/Stat- Inj Piptaz 2.25 gm /IV / TID
* dialysis was done in this patient in the view of refractory metabolic acidosis















Comments
Post a Comment