A 40 YR OLD MAN WITH SHORTNESS OF BREATH , JAUNDICE & REDUCED URINE OUTPUT
Hyndavi Konakanchi, 8th semester
Roll no: 63
October 16, 2021
A CASE DISCUSSION ON CHRONIC LIVER FAILURE AND KIDNEY INJURY
I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
Following is the view of my case :
CASE PRESENTATION:
A 40 yr old male patient came to the casualty with CHEIF COMPLAINTS of shortness of breath worsening since 2 hrs ( GRADE 3-4 ) , palpitations, bilateral pedal edema - pitting type since 10-15 days , Abdominal distension & decreased urine output since 15 days , history of fever 1 week back now it was subsided.
HISTORY OF PRESENT ILLNESS:
## Normal routine before this catastrophe , of this 40 year old gentle man was waking up at 6 am and eat food ( rice & curry ) — goes to do work related to agriculture (paddy field worker ) and daily wage worksby 8am — lunch ( rice & curry ) at 2/3 pm — resume work — comes home by 5-6 pm in the evening— takes bath & have dinner ( rice & curry ) — goes with friends outside and have toddy and whiskey — comes home by 9pm .
* He studied 10th class
* He has mixed diet and his married life was 10 yrs , the interaction with the family( wife , two sons : one aged 8 yrs and other 1 1/2 yrs ) was good and he has adequate sleep .
Patient was apparently asymptotic 6 months back ,
One day (6 months back) when he was lifting bricks ; he experienced shortness of breath for the first time and also he noticed some pedal edema
— for which he visited local doctor and was releived of his symptoms and he was diagnosed to have LIVER FAILURE ? ,with yellowish discolouration of eyes and was advised medication , from then he had intermittent episodes of SOB on doing work and continued medication.
* From 6 months his routine remained unchanged ( except he used to take rest and medication when there is an episode of SOB , on doing work ) and he stopped drinking alcohol with his friends , instead of that he spent some quality time with the family.
** But now on presentation ; he developed sever SOB ( grade 3-4 ) again on doing work in the field .
* History of pedal edema, in both lower limbs since 10-15 days which is incidious in onset and gradual in progression and worsened to the present size.
* History of abdominal distension, since 10-15 days which is progressively increasing.
* Endoscopy was done and grade 1 varices are present and ultrasound showing mild splenomegaly.
* History of decreased urine output since 10-15 days, with normal stream & post voidal residue with urgency and hesitency present.
## Now his routine changed to an extent that he can’t even walk properly with out developing SOB , so he stopped doing his agricultural and other works, now although he is waking up at 6 am ; he is taking rest , he is having decreased appetite & sleep was normal , family interactions are healthy. The financial needs now ( as he stopped working ) are met by the savings of the family .
PAST HISTORY:
* He is a known case of diabetes since 6 months and was on treatment
* Not a known case of Hypertension, Asthma, TB, Epilepsy, Coronary Artery Disease.
* History of hemodialysis in outside hospital in the view of metabolic acidosis and decreased urine output.
PERSONAL HISTORY:
* Appetite: decreased
* Diet: mixed
* Sleep : adequate
* Bowel and bladder movements: ## Regular bowel movements but,
## Has decreased micturition since 10-15 days
* Additions: * History of toddy intake since 16 years of age & whisky and brandy 90-180 ml since 10-12 years.
FAMILY HISTORY:
* Not significant
GENERAL EXAMINATION:
Patient is conscious coherent and cooperative.
He is well oriented to time, place and person.
He is moderately built and well nourished.
VITALS:
Temperature: Afebrile
Pulse Rate: 78 beats per minute
Blood pressure: 90/80 mm of Hg
Respiratory Rate: 24 cycles per minute
SpO2: 94-96 % on room air
Pallor : present
Icterus : present (mild )
No Cyanosis
No Clubbing
No Lymphadenopathy
Edema : present
SYSTEMIC EXAMINATION:
1) Abdominal examination:
Inspection:
* Shape of the abdomen: distended
* Umbilicus: slit shaped
* No visible pulsations
* Movements of abdominal quadrants with respiration are not appreciated .
* No visible scars.
Palaption:
* No local rise of temperature
* No tenderness
* No palpable masses found
* Liver and spleen are not palpable
Percussion :
* Shifting dullness : present
* Liver span: normal
Ascultation:
* bowel sounds are heard.
2) Respiratory system:
* Bilateral Air entry present
* Normal vesicular breath sounds are heard
* Position of trachea : central
* No wheeze, no crepts
3) CVS:
* S1 and S2 heart sounds are heard
*No murmurs
4) CNS:
* No abnormality detected
INVESTIGATIONS :
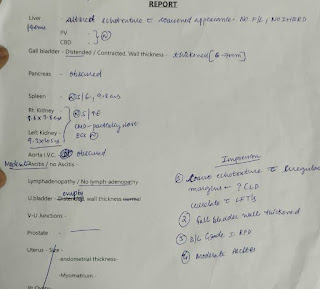
RFT , LFT , HEMOGRAM , CUE , ECG , USG - Abdomen , BGT , ABG , VIRAL SEROLOGY , CHEST X RAY, 2D echo.




















Comments
Post a Comment