Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A): 1) Shortness of breath grade 2 since 20 years( exacerbations once in a year)
* Increased frequency & severity of exerbations since 12 years.
2) Diabetes type 2 since 8 years.
3) Anemia 5 years back and treated with iron sucrose.
4) Generalised weakness and shortness of breath grade 2 since 30 days.
5) Hypertension since 20 days.
6) Pedal edema and facial puffiness since 15 days.
7) Shortness of breath grade 4 & decreased urine output since 2 days.
ANATOMICAL LOCALISATION:
* Lungs- COPD : SOB Grade II
* COPD - PAH - RHF - Pedal edema : SOB Grade IV
PRIMARY ETIOLOGY:
* Here ; in this patient it may be due to COPD (BIOMASS EXPOSURE)
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A) * Augmentin:
* Azithromycin:
* Hydrocortisone:
* Budecort nebulization:
* Ipravent: Anticholinergic bronchodilator
* Pulmoclear : Acebrophylline + Acetylcysteine
* Acebrophylline: Airway mucus regulator with antiinflammatory action.
* Acetylcysteine: Reduce the viscosity of sputum facilitating the removal of pulmonary secretions
NON PHARMACOLOGICAL INTERVENTIONS:
1.Head end Elevation:
## Significantly increases global and regional end-expiratory lung volume. It has also been shown to improve oxygenation and hemodynamic performance.
2.BiPAP:
## By having a custom air pressure for when you inhale and a second custom air pressure when you exhale, the machine is able to provide relief to your overworked lungs and chest wall muscles.
To correct respiratory acidosis
3.Chest physiotherapy:
## It is a term used for a group of treatments designed to improve respiratory efficiency, promote expansion of the lungs, strengthen respiratory muscles, and eliminate secretions from the respiratory system.It includes postural drainage, chest percussion, chest vibration, turning, deep breathing exercises, and coughing.
3) What could be the causes for her current acute exacerbation?
A) * It may be due to some bacterial / viral illness / pollutants
4. Could the ATT have affected her symptoms? If so how?
5.What could be the causes for her electrolyte imbalance?
A) ## COPD : the disease process it self may lead to electrolyte imbalance.
HYPONATREMIA in patients with COPD : developed secondary to many reasons, such as development or worsening of hypoxia, hypercapnia, and respiratory acidosis, and right-side heart failure with development of lower limb edema, renal insufficiency, use of diuretics, Syndrome of Inappropriate Antidiuretic Hormone Synthesis, malnutrition, and poor intake during acute exacerbations are common contributing factors in such patients. Activation of the renin-angiotensin-aldosterone system and inappropriately elevated plasma arginine vasopressin in COPD may aggravate the electrolyte imbalance during acute exacerbation of COPD.
HYPOCHLORAEMIA in patients with COPD:
2)Neurology (10 Marks)
A) Link to patient details:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A) *Symptomatology and event timeline:
1) Patient was a chronic alcoholic since 12 years.
2) Diabetes since 2 years ( irregular medications ).
3) 2-3 episodes of seizures in last 1 year.
4) Irrelevant talking , forgetfullness and decreased food intake since 9 days.
* Anatomical localisation:
## Here in this patient the anatomical localisation is ;
1) Brain : WERNICKE’S ENCEPHALOPATHY
2) Kidney: AKI
* Primary etiology:
## ALCOHOL
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A) 1)IVF NS and RL @150ml/hr
Indication: For dehydration
Efficacy: Highly effective, for severe dehydration
2) Inj. 1amp THIAMINE in 100ml NS, TID
MOA: Thiamine is necessary to provide energy to the CNS, helps in conduction of nerve signals.
Indication: Since Wernicke syndrome (deficiency of B1 vitamin) is a differential diagnosis.
Efficacy: Highly effective in treating B1 deficiency
3) Inj. Lorazepam
Indication: Used to sedate patient
Efficacy: High efficacy
4) T. Pregabalin 75mg/PO/ BD
MOA: Acts by releasing GABA
Indications: in seizures
Efficacy: Newer antiepileptic, good efficacy with fewer side effects
5) Inj. HAI S.C.- premeal
MOA: Short- acting insulin
Indications: Diabetes Mellitus
Efficacy: Effective for short periods of time
6) GRBS 6th hourly, premeal: 8am, 2pm, 8pm,2am
7) Lactulose 30ml/PO/BD
8) Inj 2 ampoule KCl (40mEq) in 10 NS over 4 hours
9) Syp Potchlor 10ml in one glass water/PO/BD
MOA: Potassium to increase serum K levels
Indications: in hypokalemia
Efficacy: Highly effective
3) Why have neurological symptoms appeared this time, that were absent during withdrawal earlier? What could be a possible cause for this?
A) * In this case ; the neurological symptoms are absent earlier because it is simply alcohol withdrawal.
* But now ; the patient got the neurological symptoms may be because of :
1) WERNICKE’S ENCEPHALOPATHY (or)
2) UREAMIC ENCEPHALOPATHY
4) What is the reason for giving thiamine in this patient?
A) * Here patient had developed thiamine deficiency due to chronic alcolism ; and it caused wernicke’s encephalopathy so thiamine supplemention will cause improvement of symptoms and complete resolution of symptoms in some cases.
5) What is the probable reason for kidney injury in this patient?
A) 1) Alcohol is a osmotic diuretic!
2) So causes dehydration…
3) Hence it is a pre-renal cause of AKI ( Acute kidney Injury )
6) What is the probable cause for the normocytic anemia?
A) Alcohol abuse and dependence can cause anemia through:
1) Decreased red blood cell production in the bone marrow - normocytic , normochromic anaemia.
2) Loss of blood through ulcers and inflammation - iron deficiency anemia in early stages ( normocytic normochromic anemia ).
3) Destruction of RBC’s from heart valve issues , inflammation, immune system damage , or a cancerous tumour ( normocytic normochromic anemia ).
7) Could chronic alcoholism have aggravated the foot ulcer formation? If yes, how and why?
A) * Chronic alcoholism can cause foot ulcer formation and delyaed healing peripheral neuropathy ( Alcoholic neuropathy ) , malnutrition.

B) Link to patient details:
Questions-
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A) EVOLUTION OF SYMPTOMATOLOGY IN TERMS OF EVENT TIMELINE:
1) 7days back - patient gave a history of giddiness that started around 7 in the morning; subsided upon taking rest; associated with one episode of vomiting.
2) 4 days back - patient consumed alcohol; he developed giddiness that was sudden in onset, continous and gradually progressive . It increased on standing and while walking.
3) History of postural instability- falls while walking.
** Associated with bilateral hearing loss, aural fullness, presence of tinnitus
** Associated vomiting : 2-3 episodes per day, non projectile , non bilious without food particles.
4) Present day of admission- Slurring of speech, deviation of mouth that got resoved in the same day
ANATOMICAL LOCALISATION:
* There is a presence of an infarct in the inferior cerebellar hemisphere of the brain
PRIMARY ETIOLOGY:
* Ataxia is the lack of muscle control or co-ordination of voluntary movements ,such as walking or picking up objects.
## This is usually a result of damage to the cerebellum ( part of brain that controls muscle co-ordination )
* Acute infarct in right inferior cerebellar hemisphere
## Risk factors in this patient :
Alcohol / Smoking/ Denovo HTN.
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A) A) TAB VERTIN 8mg:
*This is betahistine, which is an anti- vertigo medication
MOA-
## It is a weak agonist on H1 receptors located on blood vessels of the inner ear. This leads to local vasodilation and increased vessel permeability.
* This can reverse the underlying problem.
INDICATIONS:
* Prescribed for balance disorders.
## In this case it is used due to patients history of giddiness and balance issues.
B) TAB ZOFER 4 mg:
*This is ondanseteron- It is an anti emetic
MOA-
## It is a 5H3 receptor antagonist on vagal afferents in the gut and they block receptors even in the CTZ and solitary tract nucleus.
INDICATIONS:
* Used to control the episodes of vomiting and nausea in this patient.
C) TAB ECOSPRIN 75mg:
* This is aspirin. It is an NSAID.
MOA-
## They inhibit COX-1 and COX-2 thus decreasing the prostaglandin level and thromboxane synthesis.
INDICATIONS:
* They are anti platelet medications and in this case used to prevent formation of blood clots in blood vessels and prevent stroke.
D) TAB ATORVOSTATIN 40mg :
* This is a statin.
MOA-
## It is an HMG CoA reductase inhibitor and thus inhibits the rate limiting step in cholesterol biosynthesis. It decreases blood LDL and VLDL, decreases cholesterol synthesis, thus increasing LDL receptors in liver and increasing LDL uptake and degeneration. Hence plasma LDL level decreases.
INDICATIONS:
* Used to treat primary hyperlipidemias.
# In this case it is used for primary prevention of stroke.
E) CLOPIDOGREL 75 mg:
* It is an antiplatelet medication
MOA-
## It inhibits ADP mediated platelet aggregation by blocking P2Y12 receptor on the platelets.
INDICATIONS:
* In this case it decreases the risk of heart disease and stroke by preventing clotting
F) THIAMINE:
* It is vitamin B1
*It is naturally found in many foods in the human diet.
## In this case, the patient consumes excess alcohol- so he may get thiamine deficiency due to poor nutrition and lack of essential vitamins due to impaired ability of the body to absorb these vitamins.
INDICATIONS:
* Given to this patient mainly to prevent Wernickes encephalopathy- that can lead to confusion, ataxia and opthalmoplegia.
G) Tab MVT:
* This is methylcobalamin
*Mainly given in this case for vitamin B12 deficiency.
3) Did the patients history of denovo HTN contribute to his current condition?
A) * In this case ; yes the patient present condition of having ischemic stroke is because of his Hypertension!
4) Does the patients history of alcoholism make him more susceptible to ischaemic or haemorrhagic type of stroke?
A) * Mild to moderate intake of alcohol actually has the protective role in ischemic stroke.
* Heavy alcohol consumption is associated with the increased risk of haemorrhagic stroke.
*Recent heavy alcohol consumption can increase risk for all major types of stroke.
## The pathophysiologic mechanisms by which alcohol triggers the onset of spontaneous intracerebral hemorrhage, aneurysmal subarachnoid hemorrhage and ischemic brain infarction remain largely unresolved.
C) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A) Symptomatology & event timeline:
B/l pedal edema since 8 months
!
Dragging type of pain in left UL ass with tingling & numbness
!
Chest pain , palpitations & SOB grade-III since 5 days
Anatomical localization:
Based on the clinical history & limited investigations (ECG not available)
Heart - ? NSTEMI
Primary etiology:
? CAD
2) What are the reasons for recurrence of hypokalemia in her? Important risk factors for her hypokalemia?
A) * Based on the limited data available it is difficult to know the cause of recurrent hypokalemia in this patient.
## Further evaluation should be done.
DIAGNOSTIC APPROACH TO HYPOKALEMIA:
3) What are the changes seen in ECG in case of hypokalemia and associated symptoms?
A) ECG changes:
Symptoms &signs:
D) Link to patient details:
QUESTIONS:
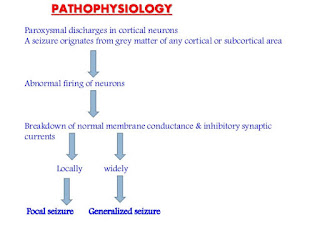
1. Is there any relationship between occurrence of seizure to brain stroke. If yes what is the mechanism behind it?
A) * Going by the history, in this patient seizures are secondary to CVA ( cerebro vascular accident )
Mechanism:
2. In the previous episodes of seizures, patient didn't loose his consciousness but in the recent episode he lost his consciousness what might be the reason?
A) Going by the history;previous episodes may be simple partial seizures predominantly involving left side ( focal seizures with no loss of consciousness) and now the recent episodes may be GTCS with loss of consciousness.
Mechanism of impairment of consciousness in seizures
* In GTCS ; there is increased activity in fronto- parietal association cortex and related subcortical structures is associated with the loss of consciousness & there is an abnormal decreased activity in the same networks may cause loss of consciousness in complex partial seizures
E) Link to patient details:
Questions:
1) What could have been the reason for this patient to develop ataxia in the past 1 year?
A) Going by the history here in this patient; he is a chronic alcoholic & ataxia may be due to cerebellar degeneration or peripheral neuropathy.
2) What was the reason for his IC bleed? Does Alcoholism contribute to bleeding diatheses ?
A) * Coming to the reason of his IC bleed ; it can be because of his hypertension or trauma
# Going by the history; there is no recent fall ( trauma )
## He is not a known case of hypertension either but; according to:
SOKOLOW-LYON CRITERIA:
# S wave in V1 and R wave in V5/ V6 values in ECG are more than 35 mm suggestive of left ventricular hypertrophy secondary to undiagnosed chronic HTN)
Conclusion:* In this patient based on the data available IC bleed may be secondary to previously undiagnosed HTN. (Or) * Chances of hemorrhage due to heavy alcohol consumption are also present…
* Alcohol and bleeding diathesis; Alcohol ( ethanol ) intake has effects on platelet aggregation and activation, coagulation factors including von Willebrand factor (vWF) , and the fibrinolytic system.
* With regard to the effect of alcohol on platelet function , evidence in the literature suggests both platelet activation and platelet inhibition by ethanol. A unifying hypothesis is that platelets are partially activated by ethanol, with partial degranulation allowing for continued circulation of platelets with impaired function.
## Evidence also exists showing that ethanol also exists showing that ethanol decreases fibrinogen, factor VII, and vWF levels.
* In addition, alcohol intake has been found to increase fibrinolysis by increasing tissue plasminogen activator activity
F) Link to patient details:
Questions:
1.Does the patient's history of road traffic accident have any role in his present condition?
A) * No ,it was alcohol drinking and emotional disturbance of the patient that led to his situation.
*Road traffic accident only led to dislocation of shoulder , zygomatic & mandibular process.
2.What are warning signs of CVA?
A) WARNING SIGNS OF CVA:
3.What is the drug rationale in CVA?
A) 1. Injection MANNITOL 100ml IV TD :- Because of its osmotic effect, mannitol is assumed to decrease cerebral edema.
•Mannitol might improve cerebral perfusion by decreasing viscosity, and as a free-radical scavenger, it might act as a neuroprotectant.
2. TAB. ECOSPRIN 75 mg po OD :- Aspirin, which thins the blood and thereby prevents clots, is currently used to reduce the long-term risks of a second stroke in patients who've had an ischemic stroke.
• But giving aspirin to patients who've had a hemorrhagic stroke is considered dangerous, as it can cause more bleeding and more damage.
3. TAB ATORVAS 40mg po HS :-Statins, inhibitors of HMG-CoA reductase, are widely used cholesterol-lowering drugs and reduce the incidence of myocardial infarctions and stroke.
4. Does alcohol has any role in his attack?
A) * Mild to moderate intake of alcohol actually has the protective role in ischemic stroke.
* Heavy alcohol consumption is associated with the increased risk of haemorrhagic stroke.
## Yes alcohol has a role in his attack … patient was occasionally alcoholic who used to drink 500 ml of alcohol (whiskey) once in week!
5.Does his lipid profile has any role for his attack?
A) *No in this case the lipid profile is normal and it has no role in his attack…
G) Link to patient details:
Questions:
1)What is myelopathy hand ?
A) A characteristic dysfunction of the hand has been observed in various cervical spinal disorders when there is involvement of the spinal cord.
* There is loss of power in the adduction and extension of the ulnar two or three fingers and an inability to grip and release rapidly with these fingers .
## These changes have been termed “ myelopathy hand”
2)What is finger escape ?
A) # It is known as Wartenberg’s sign :
* It is a neurological sign consisting of involuntary abduction of fifth finger ( little finger ) , caused by unopposed action of the extensor digiti minimi.
## This finding of weak finger adduction in cervical myelopathy is also called “finger escape sign”.
3)What is Hoffman’s reflex?
A) procedure: The test is done by tapping or flicking the nail of the middle finger to produce the flexion of the index finger to the thumb.
Interpretation: If the reflex is positive ; it indicates the possible existence of spinal cord compression from a lesion on the spinal or another underlying nerve condition.
H) Link to patient details:
Possible questions:
1) What can be the cause of her condition ?
A) * Here in this patient; seizures may be caused by CORTICAL VEIN THROMBOSIS ( seen on MRI )
2) What are the risk factors for cortical vein thrombosis?
A) Risk factors for CVT :
1) INFECTIONS:
* Meningitis, otitis , mastoiditis
2) PROTHROMBOTIC STATES:
* Pregnancy, puerperium, antithrombin deficiency, protein c & s deficiency, Hormone replacement therapy.
3) MECHANICAL:
* Head trauma, Lumbar puncture.
4) INFLAMMATORY:
* SLE, Sarcoidosis, Inflammatory bowel disease.
5) MALIGNANCY
6) DEHYDRATION
7) NEPHROTIC SYNDROME
8) DRUGS:
* Oral contraceptives, steroids, Inhibitors of angiogenesis.
9) CHEMOTHERAPY:
* Cyclosporine and L asparginase.
10) HEMATOLOGICAL:
* Myeloproliferative Malignancies
* Primary and secondary polycythemia
11) INTRACRANIAL:
* Dural fistula
* Venous anomalies
12) VASCULITIS :
* Behcets disease wegner’s granulomatosis
3)There was seizure free period in between but again sudden episode of GTCS why?resolved spontaneously why?
A) * Here initially patient was completely sedated with medazolam infusion and acheived a seizure free period and followed by 1-2 episodes of recurrence after tapering the dose of medazolam ( benzodiazepine drug )
4) What drug was used in suspicion of cortical venous sinus thrombosis?
A) * Anticoagulants are used for the prevention of harmful blood clots.
* Here in this patient; CLEXANE ( enoxaparin ) low molecular weight heparin binds and potentiates anti thrombin 3 , a serine protease inhibitor to form complex and irreversibly inactivates factor xa.
3) Cardiology (10 Marks)
A) Link to patient details:
1.What is the difference btw heart failure with preserved ejection fraction and with reduced ejection fraction?
A)
2.Why haven't we done pericardiocenetis in this pateint?
A) * This patient had no cardiac tamponade which is an absolute indication for pericardiocentesis.
## So we treated him conservatively considering the risks associated with the procedure.
## If he had developed cardiac tamponade at any point of time we would have immediately done a pericardiocentesis.
3.What are the risk factors for development of heart failure in the patient?
A) Here;
* This patient has most of the risk factors for heart failure like:
Old age
T2DM
HTN
CAD
Smoking
Alcohol
4.What could be the cause for hypotension in this patient?
B) Link to patient details:
Questions:
1.What are the possible causes for heart failure in this patient?
A) POSSIBLE CAUSES :
Old age
T2DM
HTN
Alcohol
CAD
CKD
2.what is the reason for anaemia in this case?
A) *Anemia of chronic disease
CKD & ANEMIA:
CHRONIC HEART FAILURE & ANEMIA:
CKD < > HEART FAILURE < > ANEMIA : All these are interlinked with each other.
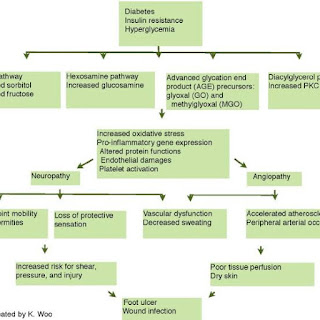
3.What is the reason for blebs and non healing ulcer in the legs of this patient?
A) * DIABETES
4. What sequence of stages of diabetes has been noted in this patient?
A) * This patient is in stage-IV T2DM with established end stage micro & macro vascular complications.
C) Link to patient details:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A) Symptomatology & event timeline:
Chronic alcoholic
!
NSAID abuse since 3 yrs
!
Facial Puffiness on & off since 2-3 yrs
!
HTN since 1 year
!
SOB grade : II - IV & decreased urine output since 2 days
!
Anuria since 1 day
!
Denovo DM
Anatomical localization:
Kidney : CKD (?Analgesic Nephropathy)
Heart : HFrEF (?CAD)
Primary etiology:
NSAID abuse
CKD
HTN
T2DM
CAD
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A) 1. TAB.DYTOR
Mechanism: Through its action in antagonizing the effect of aldosterone, spironolactone inhibits the exchange of sodium for potassium in the distal renal tubule and helps to prevent potassium loss.
2. TAB.ACITROM
Mechanism: Acenocoumarol inhibits the action of an enzyme Vitamin K-epoxide reductase which is required for regeneration and maintaining levels of vitamin K required for blood clotting
3. TAB. CARDIVAS
Mechanism:Carvedilol works by blocking the action of certain natural substances in your body, such as epinephrine, on the heart and blood vessels. This effect lowers your heart rate, blood pressure, and strain on your heart. Carvedilol belongs to a class of drugs known as alpha and beta-blockers.
4. INJ. HAI S/C
Mechanism: Regulates glucose metabolism
* Insulin and its analogues lower blood glucose by stimulating peripheral glucose uptake, especially by skeletal muscle and fat, and by inhibiting hepatic glucose production; insulin inhibits lipolysis and proteolysis and enhances protein synthesis; targets include skeletal muscle, liver, and adipose tissue.
5.TAB. DIGOXIN
Meechanism: Digoxin has two principal mechanisms of action which are selectively employed depending on the indication:
Positive Ionotropic: It increases the force of contraction of the heart by reversibly inhibiting the activity of the myocardial Na-K ATPase pump, an enzyme that controls the movement of ions into the heart.
3) What is the pathogenesis of renal involvement due to heart failure (cardio renal syndrome)? Which type of cardio renal syndrome is this patient?
4) What are the risk factors for atherosclerosis in this patient?
A) Old age
Male gender
Alcohol
HTN
T2DM
CKD
5) Why was the patient asked to get those APTT, INR tests for review?
A) ## Patient was kept on T.ACITROM (ACENOCOUMARAL) which is an anti coagulant and was discharged.
* So to moniter the response to treatment & maintain it within a therapeutic range, to provide the benefits of anticoagulation, while avoiding the risks of haemorrhage PT , INR & APTT are monitored frequently.
D) Link to patient details:
Questions-
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A) Symptomatology & event timeline:
T2DM since 12 yrs
!
On & off chest pain since 1 year
!
TB 7 months back - used ATT for 6 months
!
HTN since 6 months
!
Profuse sweating & SOB grade : III - IV since 30 min
Anatomical localization:
Heart : CAD : NSTEMI
Primary etiology:
T2DM & HTN - CAD
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A) TAB MET XL contains :
* Metoprolol as active ingredient
MOA: cardioselective beta blocker
Beta blockers work by blocking the effects of the hormone epinephrine, also known as adrenaline. Beta blockers cause your heart to beat more slowly( negative chronotropic effect)
and with less force( negative inotropic effect). Beta blockers also help open up your veins and arteries to improve blood flow.
Indications: it is used to treat Angina, High blood pressure and to lower the risk of hear attacks.
3) What are the indications and contraindications for PCI?
A) INDICATIONS:
Acute ST-elevation myocardial infarction (STEMI)
Non–ST-elevation acute coronary syndrome (NSTE-ACS)
Unstable angina.
Stable angina.
Anginal equivalent (eg, dyspnea, arrhythmia, or dizziness or syncope)
High risk stress test findings.
CONTRAINDICATIONS:
Intolerance for oral antiplatelets long-term.
Absence of cardiac surgery backup.
Hypercoagulable state.
High-grade chronic kidney disease.
Chronic total occlusion of SVC.
An artery with a diameter of <1.5 mm.
4) What happens if a PCI is performed in a patient who does not need it? What are the harms of overtreatment and why is research on overtesting and overtreatment important to current healthcare systems?
A) * Over diagnosis is which occurs when a true abnormality is discovered , but the detection of that abnormality and its treatment doesn’t benefit the patient.
* Over diagnosis will lead to over treatment , psychological effects & economic burden.
To prevent these adverse events more research is important in this over diagnosis & over treatment.
E) Link to patient details:
Questions:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A) EVOLUTION OF THE SYMPTOMATOLOGY:
* Here in this patient;
1) CHEST PAIN since 3 days.
2) GIDDINESS since morning.
3) PROFUSE SWEATING since morning.
ANATOMICAL LOCALISATION:
* Lesion in the inferior wall of the heart.
PRIMARY ETIOLOGY:
Diabetics Mellitus
Hypertension
2) What are mechanism of action, indication and efficacy over placebo of each of the pharmacological and non pharmacological interventions used for this patient?
A) MECHANISM OF ACTION, EFFICACY OF PHARMACOLOGICAL & NON-PHARMACOLOGICAL INTERVENTION USED:
* ANTIPLATELETS: ASPIRIN + CLOPIDOGREL
* STATINS:
*PTCA:
CLINICAL INDICATIONS OF PTCA:
* Acute ST - elevation myocardial infarction ( STEMI )
* Non ST - elevation acute coronary syndrome ( NSTE-ACS )
* Unstable angina
* Stable angina
* Anginal equivalent (eg; dyspnoea, arrhythmia, or dizziness or syncope )
* High risk stress test findings.
3) Did the secondary PTCA do any good to the patient or was it unnecessary?
A) ## The secondary PTCA was unnecessary in the patient as he already crossed the window period of 12 hours and was doing fine without PTCA.
F) Link to patient details:
1. How did the patient get relieved from his shortness of breath after i.v fluids administration by rural medical practitioner?
A) * Here the history itself is not clear like what was given and he may have given some diuretic also which decreased his SOB.
## Clearly its not the IV FLUIDS which releived his SOB.
2. What is the rationale of using torsemide in this patient?
A) * Torsemide : loop diuretic.
## This patient is in fluid overload & heart failure where diuretics are the main stay of treatment (reducing preload)
3. Was the rationale for administration of ceftriaxone? Was it prophylactic or for the treatment of UTI?
A) * No its not prophylactic.
## H/o whitish discharge & TLC was 18000 which clearly indicates infection for which ceftriaxone was given.
4) Gastroenterology (& Pulmonology) 10 Marks
A) Link to patient details:
QUESTIONS:
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A) *Evolution of patient symptomatology:
1) He is alcoholic since 9 years.
2) His symptoms of pain abdomen and vomitings started from 5 yrs and got conservative treatment.
3) Following that ; he stopped alcohol intake for 3 years and remained symptom free.
4) Later he again developed symptoms due to starting alcohol intake.(5-6 episodes in last year)
5) From past 20 days ; he drastically increased his alcohol consumption (5 bottles of toddy per day).
6) Last binge of alcohol 1 week back following which he again has pain abdomen and vomiting from 1 week and fever from 4 days.
7) Then he developed constipation and passing flatus since 4 days.
8) He also developed burning micturition since 4 days.
9) He got admitted in hospital and got treated conservatively for 4 days
10) Inspite; patient is clinically deteriorating with SIRS.
11) Malecot drain is placed for pseudocyst and peripancreatic collections.
12) ICD placed for the left sided hydropneumothorax
13) Escalation of antibiotics & other symptomatic treatment continued.
14) Clinical improvement with resolution of symptoms and discharged 10 days later.
*Anatomical localisation:
## Here in this case anatomical localisation is PANCREAS & LUNG.
* Primary etiology:
## Here in this case ; primary etiology is ALCOHOL INTAKE!
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
A) Efficacy of drugs used :
* P: 302 patients from 32 hospitals ( moderate - severe pancreatitis ).
* I: Group 1 (n : 98 ) and Group 2 ( n : 101 ) received 100 mg and 200 mg respectively.
* C: Group P received placebo.
* O: No significant differences among treatment groups ; with respect to :
# Respect to mortality.
# Rate of newly developed complications.
# Duration of pain.
# Surgical interventions.
# Length of the hospital stay.
2) PANTOP:
* P : 40 patients with acute pancreatitis
* I : Group - A : Given pantoprazole 40mg BD
* C : Group - B : Not given pantop
* O : No significant difference in clinical course or outcome.
## In an experimental study with rats it shows PPZ possesses anti-inflammatory in vivo properties and attenuates the course of AP. This is mediated via a reduced expression of inflammatory and adhesive proteins with a consecutive decrease in platelet and leukocyte activation as key steps in the pathogenesis of AP.
3) PERCUTANEOUS DRAINAGE:
* Early and aggressive intervention helps reduce the morbidity and mortality by preventing the evolution of MODS.
## Percutaneous catheter drainage can be a primary treatment option for necrotizing pancreatitis. In addition, it helps to stabilize critically ill patients and delay the surgical procedure to beyond 4 weeks to improve the surgical outcomes.
4) TPN:
* Positively affect the course of the disease and improves the outcome.
5) FLUID MANAGEMENT:
* Fluid therapy has the potential to reduce the progression of pancreatic necrosis and its associated risk of mortality.
## Even I as a treating physician will appraoch ; the same followed by the treating team; I would like to follow up the patient witn MRCP and CYSTOGASTROSTOMY…
B) Link to patient details:
1) What is causing the patient's dyspnea? How is it related to pancreatitis?
A) * Here ; in this patient he developed bilateral mild pleural effusion, as a complication of pancreatitis due to formation of pancreatico pleural fistula…
## So this pleural effusion, may be the cause of his dyspnoea.
2) Name possible reasons why the patient has developed a state of hyperglycemia.
A) * Hyperglycaemia may be because of his pancreatitis…
MECHANISM:

3) What is the reason for his elevated LFTs? Is there a specific marker for Alcoholic Fatty Liver disease?
A) * Here in this patient; elevated LFT maybe contributed to his alcohol consumption and developing Alcohol Fatty liver disease.

## Specific marker of ALCOHOL FATTY LIVER DISEASE:
* Liver disease is the most likely diagnosis if the AST level is more than twice that of ALT , a ratio some studies have found in more than 80 percent of alcoholic liver disease patients . An elevated level of the liverenzyme GGT is another gauge of heavy alcohol use and liver injury.
4) What is the line of treatment in this patient?
For the master chart to the "pancreatitis thesis project" please get in touch with Dr Shashikala PGY1 and Dr Divya PGY2 and share their insights into the above project problem they are working on.
C) Link to patient details:
Possible Questions :-
1) what is the most probable diagnosis in this patient?
A)* Ruptured liver abscess
*Organized collection secondary to hollow viscous perforation.
2) What was the cause of her death?
A) * May be SEPSIS with MODSdue to ruptured liver abcess…
# But again etiology ; can be confirmed only by exploratory laporotomy.
3) Does her NSAID abuse have something to do with her condition? How?
A) * If at all it is a hollow viscous perforation it can be secondary to her NSAID abuse.
She had grade-3 RPD changes in right kidney
She may be having underlying CKD which is secondary to her NSAID abuse (Analgesic nephropathy)

5) Nephrology (and Urology) 10 Marks
A) Link to patient details:
1. What could be the reason for his SOB ?
A) * His SOB was caused due to ACIDOSIS caused by diuretics.
2. Why does he have intermittent episodes of drowsiness ?
A) HYPONATREMIA was the cause for his drowsiness.
3. Why did he complaint of fleshy mass like passage in his urine?
A) * Plenty of pus cells in his urine passage appeared as fleshy mass like passage to him.
4. What are the complications of TURP that he may have had?
A) * DIFFICULTY MICTURITION
* INFECTION
* ELECTOLYTE IMBALANCE
B) Link to patient details:
Questions
1.Why is the child excessively hyperactive without much of social etiquettes ?
A) * Here in this case ;the child seems to be psychosomatic , hence the behaviour…
2. Why doesn't the child have the excessive urge of urination at night time ?
A) * Here ; the child has excessive urge to urinate during day time even though bladder isn’t full; because of his psychological impulse to urinate.
* During night time; he wouldn’t have compulsion to do so since he’s asleep…
## Here; cause of overactive bladder is a condition called pollakiuria, or frequent daytime urination syndrome. Children who have pollakiuria urinate frequently. In some cases, they may urinate every five to 10 minutes or urinate between 10 and 30 times a day. This condition is most common among children aged 3 to 8 and is present only during waking hours. There are no other symptoms present. Doctors believe that pollakiuria is related to stress.
3. How would you want to manage the patient to relieve him of his symptoms?
A) * I wouldn’t recommend any medications as such because all the reports, clinical findings seem to be normal.
* I will counsell him mentally and go to therapy to overcome his psychological compulsion to urinate excessive amount of times , even when he doesn’t need to!
# It is usually unnecessary to treat pollakiuria. The symptoms should subside within a few weeks of starting. In some cases, however, it may take 7-12 months to clear up completely.
* It is also helpful to try to identify possible triggers. A trigger could be anything that causes the child stress.
## Currently, there are no medications that help with pollakiuria , a placebo may be of help…
6) Infectious Disease (HI virus, Mycobacteria, Gastroenterology, Pulmonology) 10 Marks
A) Link to patient details:
Questions:
1.Which clinical history and physical findings are characteristic of tracheo esophageal fistula?
A) * In this patient; CLINICAL HISTORY:
* Cough on taking foods and liquids which was initially non productive then associated with sputum which is white in colour and non foul smelling.
* Difficult in swallowing since 2 months with solids and liquids. Patient is on RT feeding.
* History of weight loss and SOB
* One episode of vomiting
* Fever episodes
PHYSICAL FINDINGS:
*Thinly built and malnourished
* Respiratory system examination: Wheeze present in bilateral mammary areas.
* Neck examination: laryngeal crepitus- positive
2) What are the chances of this patient developing immune reconstitution inflammatory syndrome? Can we prevent it?
A) * A paradoxical clinical worsening of a known condition or the appearance of a new condition after initiating antiretroviral therapy (ART) therapy in HIV-infected patients resulting from restored immunity to specific infectious or non-infectious antigens is defined as immune reconstitution inflammatory syndrome (IRIS).
* Because clinical deterioration occurs during immune recovery, this phenomenon has been described as immune restoration disease (IRD), immune reconstitution syndrome (IRS), and paradoxical reactions.
##Given the role of the host inflammatory response in this syndrome, the term (IRIS) has been proposed and has become the most widely used and accepted term to describe the clinical entity.
** However ; chances of IRIS are less…
PREVENTION:
* The most effective prevention of IRIS would involve initiation of ART before the development of advanced immunosuppression. IRIS is uncommon in individuals who initiate antiretroviral treatment with a CD4+ T-cell count greater than 100 cells/uL.
* Aggressive efforts should be made to detect asymptomatic mycobacterial or cryptococcal disease prior to the initiation of ART, especially in areas endemic for these pathogens and with CD4 T-cell counts less than 100 cells/uL.
* Two prospective randomized studies are evaluating prednisone and meloxicam for the prevention of paradoxical TB IRIS.
7) Infectious disease and Hepatology:
Link to patient details:
1. Do you think drinking locally made alcohol caused liver abscess in this patient due to predisposing factors present in it ?
A) * Amoebic liver abcess (ALA ) seen commonly in the tropics is predominantly confined to adult males, especially those who consume locally brewed alcohol, although intestinal amoebiasis occurs in all age groups and in both genders.
* It has been argued that socioeconomic factors and poor sanitary conditions are the primary culprits that casually link alcohol to ALA.
What could be the cause in this patient ?
## Hence the consumption of locally made contaminated alcohol ( toddy ) is the most likely cause of Liver abcess in this patient.
* Contaminated may be by entamoeba histolytica
* Alcohol consumption alone is never the cause for the liver abcess
2. What is the etiopathogenesis of liver abscess in a chronic alcoholic patient ? ( since 30 years - 1 bottle per day)
A) ETIOPATHOGENESIS:
3. Is liver abscess more common in right lobe ?
A) * Yes most common lobe involvement in liver abcess is right lobe .
** STREAMLINE EFFECT OF PORTAL CIRCULATION IS CAUSATIVE FACTOR!
( explained below )
## This is attributed to the fact that; right lobe is supplied predominantly by superior mesentric vein, where as the left lobe is supplied by splenic vein ; this attributes to differences in development of liver disease in both lobes…
4.What are the indications for ultrasound guided aspiration of liver abscess ?
A) INDICATIONS OF LIVER ABCESS DRAINAGE:
1) If the abcess is large ( 5cm or more ) because it has more chances to rupture.
2) If the abcess is present in left lobe as it may increase
the chances of peritoneal leak & pericardial leak.
3) If the abcess is responding to the drugs for 7 days or more days
## METHOD OF ABCESS DRAINAGE: * Aspiration done using needle or catheter under imaging.
B) Link to patient details:
QUESTIONS:
1) Cause of liver abcess in this patient ?
A) Here ; the cause of liver abcess is :
* Amoebic liver abcess (ALA ) seen commonly in the tropics is predominantly confined to adult males, especially those who consume locally brewed alcohol, although intestinal amoebiasis occurs in all age groups and in both genders.
* It has been argued that socioeconomic factors and poor sanitary conditions are the primary culprits that casually link alcohol to ALA.
## Hence the consumption of locally made contaminated alcohol ( toddy ) is the most likely cause of Liver abcess in this patient.
* Contaminated may be by entamoeba histolytica
* Alcohol consumption alone is never the cause for the liver abcess
2) How do you approach this patient ?
A) * The patient is well managed by treating team ; even me will follow the same approach; explained below:
INVESTIGATIONS:
CBP: leukocytosis
LFT : Riased ALP
RFT , URINE ANALYSIS, CHEST X- RAY: Normal
USG : Hyperechoic mass in right lobe of liver
ANALYSIS OF REPORTS & DIAGNOSIS:
*Based on right hypochondriac and epigastric pain , fever
* USG finding of hyperechoic mass in right lobe of liver along with other supportive investigations like leucocytosis ( suggestive of infection/inflammation) and ALP ( Alkaline phosphatase ) rise in LFT is a suggestive diagnosis of LIVER ABCESS.
TREATMENT ALONG WITH RATIONALE:
* INJECTION. ZOSTUM 1.5 gm IV BD (twice daily)
Zostum is a combination of drugs - SULBACTUM (pencillin) & CEFOPERAZONE(cephalosporin) [Antibiotic]: It is used here to treat if any bacterial cause ( since we can’t take the risk relying on only anti amoebic therapy)
* INJECTION. METROGYL 500mg IV TID ( thrice daily )
Metrogyl has the drug called METRONIDAZOLE [Antibiotic]: For amoebic cause
* INJECTION. OPTINEURIN 1amp in 100 ml NS( Nor
mal Saline) IV OD ( once daily)
Optineurin is a multivitamin drug { A combination of B1,B2, B3, B5,B6, B12 } given here as a supplement
* TAB. ULTRACET 1/2 QID( four times a day)
Ultracet is a combination of drugs - TRAMADOL(opiod analgesic) and ACETAMINOPHEN (analgesic and antipyretic) : Given for pain and fever
* TAB. DOLO 650 mg SOS (if needed) given for fever and pain
3) Why do we treat here ; both amoebic and pyogenic liver abscess?
A) * Considering the following factors:
1) Age and gender of patient: 21 years ( young ) and male.
2) Single abcess.
3) Right lobe involvement.
## The abcess is most likely AMOEBIC LIVER ABSCESS …
** But most of the patients with amoebic liver abcess have no bowel symptoms, examination of stool for ova and parasite and antigen testing is insensitive and insensitive and not recommended.
# And considering the risk factors associated with aspiration for pus culture:
1) Sometimes ; abcess is not accessible for aspiration if it is in posterior aspect or so.
2) Sometimes ; it has thin thinwall which may rupture if u aspirate.
3) Sometimes ; it is unliquefied.
## Due to lack of resources , we cannot confirm whether it is pyogenic / amoebic , so we treat them both emperically in clinical practice.
* Since we cannot take risk , we should however administer antibiotics also ( like in pyogenic liver abcess)
4) Is there a way to confirmthe definitive diagnosis in this patient?
A) * Yes in a high resource setting cause of liver abscess is usually determined using multiple diagnostic strategies , including blood cultures , entamoeba serology , liver abscess aspirate for culture and molecular and antigen testing.
8) Infectious disease (Mucormycosis, Ophthalmology, Otorhinolaryngology, Neurology) 10 Marks
A) Link to patient details:
Questions :
1) What is the evolution of the symptomatology in this patient in terms of an event timeline and where is the anatomical localization for the problem and what is the primary etiology of the patient's problem?
A) Symptomatology & event timeline:
HTN since 2 yrs
!
COVID-19 vaccination 15 days back
!
Fever since 10 days
!
Generalized weakness , facial puffiness & peri orbital edema since 1 week
!
Weakness of right UL & LL since 4 days
!
Altered sensorium since 2 days
!
Denovo T2DM
Anatomical localization:
Oral cavity , nose & orbit : Oro rhino orbital mucormycosis
Brain : CVA (Acute infarct in left frontal & temporal lobes)
Primary etiology:
Diabetes -- mucormycosis
Mucormycosis -- CVA (Acute infarct in left frontal & temporal lobes
2) What is the efficacy of drugs used along with other non pharmacological treatment modalities and how would you approach this patient as a treating physician?
A) AMPHOTERICIN - B
3) What are the postulated reasons for a sudden apparent rise in the incidence of mucormycosis in India at this point of time?
A) *Mucormycosis is may be being triggered by the use of steroids, a life-saving treatment for severe and critically ill COVID-19 patients.
## Steroids reduce inflammation in the lungs for Co-19 and appear to help stop some of the damage that can happen when the body's immune system goes into overdrive to fight off coronavirus. But they also reduce immunity and push up blood sugar levels in both diabetics and non-diabetic COVID-19 patients.
* With the COVID-19 cases rising in India the rate of occurrence of mucormycosis in these patients is increasing.
9) Infectious Disease (Covid 19)
As these patients are currently taking up more than 50% of our time we decided to make a separate log link here:
for this question that contains details of many of our covid 19 patients documented over this month and we would like you to:
1) Sort out these detailed patient case report logs into a single web page as a master chart
2) In the master chart classify the patient case report logs into mild, moderate severe and
3) indicate for each patient, the day of covid when their severity changed from moderate to severe or vice versa recognized primarily through increasing or decreasing oxygen requirements
4) Indicate the sequence of specific terminal events for those who died with severe covid (for example, altered sensorium, hypotension etc).
Please check out the thesis log here for the example of a blogged master chart https://vamsikrishna1996.blogspot.com/2020/10/thesis.html and please get in touch with Dr Sai Charan PGY1 who is liasing between us and the MRD for this project where we hope this data can allow us to get some clues on predicting the factors driving recovery from covid 19.
A)
LINK TO MY COVID MASTER CHART:
10) Medical Education: (10 marks)
Experiential learning is a very important method of Medical education and while the E logs of the students in the questions above represent partly their and their patient's experiences, reflective logging of one's own experiences is a vital tool toward competency development in medical education and research. A sample answer to this last assignment around sharing your experience log of the month can be seen in the link below but while this is by a student onsite in hospital and not locked down at home we would be very interested to learn about your telemedical learning experiences from our hospital as well as community patients over the last month even while locked down at home: https://onedrive.live.com/view.aspx?resid=4EF578BAE67BA469!4180&ithint=file%2cdocx&authkey=!AOy7BpRTn42DBMo 

































































Comments
Post a Comment